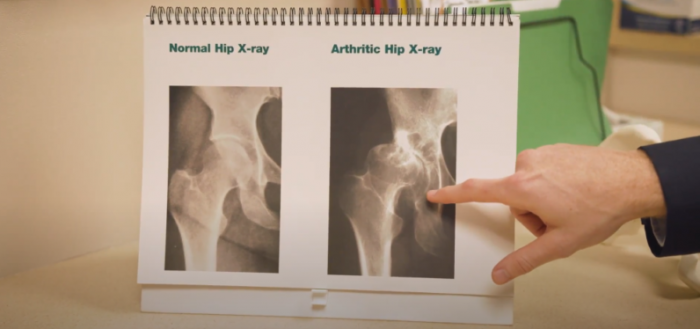
The most common type of arthritis is osteoarthritis, which affects an estimated 31 million Americans. Osteoarthritis is a gradual breakdown of cartilage in the joints. Resulting from wear and overuse, it can severely impact a person’s lifestyle. There is no cure for this disease, but the good news is that there are many treatment options available to help manage joint pain and keep you active.
In the early stages of arthritis, your doctor may recommend changing your activity level, wearing a brace, weight loss, physical therapy or and anti-inflammatory medication such as ibuprofen or acetaminophen for symptom relief. As arthritis progresses and symptoms worsen, an injection may help alleviate pain in your joints and allow you to continue with activities.
Chronic conditions, such as degenerative arthritis, can often be managed with intermittent injections. Depending on the condition and underlying pathology, many patients can maintain a pain-free lifestyle for several years by only receiving injections every three to four months. If a physician or physician assistant recommends a joint injection to help modify symptoms, improve recovery, or manage a long-term condition, the patient should be aware of both the potential benefits and limited risk factors associated with the various types of injections procedures.
Corticosteroid Injections
Corticosteroid injections are used to help reduce inflammation. For years studies have proven them to be beneficial for medium to short term use and immediate pain relief. These injections are common for joint inflammation resulting from conditions such as osteoarthritis, gout, pseudogout, and tendonitis. They are generally approved by most insurances and usually do not require pre-authorization. Corticosteroid injections are usually very well tolerated and can be done with little or no discomfort. The most common side-effects include pain or swelling at the injection site, facial flushing or redness, and a transient elevation in blood sugar levels.
Hyaluronic Acid/Gel Injections
Gel injections (Hyaluronic acid) have been approved by the FDA for use in the management of arthritis of the knee. They have been shown in several studies to reduce knee pain and inflammation associated with osteoarthritis for 6-12 months. Gel injections (hyaluronic acid) may allow some patients to remain active and delay knee replacement. Unfortunately, these injections are often not covered by insurance and must be pre-authorized. Side effects of gel injections may include pain and swelling at the injection site.
Platelet Rich Plasma (PRP) Injections
Platelet Rich Plasma (PRP) injections are derived from a patient’s blood. Blood is taken from a patient and spun in a centrifuge to obtain a layer that consists of platelet-rich plasma with or without a high concentration of white blood cells. Think of it like an injection that is trying to help the body heal itself. By injecting activated platelets into diseased tissue, the hope is that it would induce a healing response.
PRP has shown clinical promise in studies for chronic tendonitis (examples include tennis and golfer’s elbow, hamstring, or achilles tendonitis). Platelet-rich plasma injections have little to no side effect risk, although pain during and after the procedure for a short term is common. There is no clear data on the number of treatments required to maximize the effect of PRP, and it is still considered to be experimental, and thus is not covered by private insurance or Medicare. The Center attempts to limit the expense to patients, and if a patient wishes to have a PRP injection, our scheduling or insurance authorization staff will contact you directly to review the scheduling and cost of the procedure.
Stem Cell Injections
Stem cell injections are best thought of as an immature cell that has not yet developed to become a very specific cell. Some treatments have a significant risk of infection, specifically if the source of the stem cells is from outside of the patient. The injections are costly and insurance companies usually do not cover the treatment. Stem cell treatment for arthritis is not standardized and is currently under significant review and investigation by the FDA. The only true FDA approved stem cell products for use in the USA are derived from umbilical cord blood and are approved for very limited use.
Before considering receiving any stem cell therapy, we recommend reviewing the FDA website. Ask if your treatment provider has directly approved or reviewed the specific treatment or protocol or if it is a part of an Investigational Drug Application (IND) plan, which is allowed by the FDA. Orthopedic providers at The Center continue to review the latest studies for the safety and efficacy of these treatments and continue to remain optimistic that someday we will have a viable stem cell option for patients.
When you are discussing treatment options for osteoarthritis with your orthopedic doctor, keep in mind that results can vary dramatically from patient to patient. As medical research continues to develop, our doctors will guide you through the different treatment options for pain management and get you back to your daily activities.
Stay informed about upcoming webinars and events, and gain valuable insights on leading a healthy, pain-free life from our experts by subscribing to our monthly newsletter. Click the button below to join!