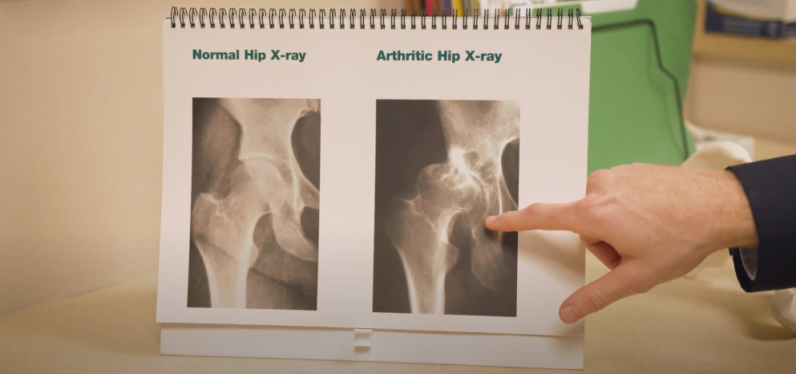
For patients with osteoarthritis or that have experienced trauma to their hip, a total hip replacement can restore function and decrease pain. This is done by replacing the damaged or diseased bone with a metal or plastic implant, which is designed to replicate a healthy hip joint. The most commonly utilized total hip replacement is the posterior approach (through the back of the hip), which has been performed successfully for decades. The anterior approach (through the front of the hip) has been utilized as long as the posterior approach but its popularity has grown in the US over the past 10-15 years.
If you are considering a total hip replacement, this guide will help compare the two approaches and give you information to discuss with your surgeon. There are risks and benefits to each type of approach. In addition, be prepared to ask your surgeon about their experience, complications, and overall outcomes. Orthopedic surgeon, Dr. Connor King, explains the differences between these two approaches in the video below.
HIP REPLACEMENT SURGERY
Posterior Approach
Posterior hip replacement, the traditional approach to hip replacement surgery, involves accessing the hip joint from the back of the body. Surgeons perform this approach by cutting through muscles and tendons to reach the hip joint. Despite its longer recovery period, posterior hip replacement remains a reliable technique, particularly for patients with complex hip conditions or prior hip surgeries.
- The majority of patients are a candidate for this type of surgery.
- The patient is positioned on his or her side during surgery.
- The surgeon makes a 4-6 inch incision just behind the hip, along the buttock area.
- The surgery takes 60-70 minutes.
- It is the most common approach and provides the greatest patient safety.
Anterior Approach
Anterior hip replacement involves accessing the hip joint from the front of the body. Surgeons perform this approach through a smaller incision and by carefully navigating between muscles and tendons. This muscle-sparing technique aims to minimize damage to surrounding tissues, potentially leading to faster recovery and improved early stability of the hip joint.
- Candidates for this approach are not significantly overweight, have no femur deformities, and normal pelvis anatomy.
- The patient is positioned on his or her back on a special surgical table so the surgeon can manipulate the leg during surgery.
- The surgeon makes a 4-6 inch incision on the upper thigh.
- The surgery takes 90-100 minutes.
- This is a technically challenging procedure. Patients should find a surgeon very experienced in this approach.
INTRAOPERATIVE VISUALIZATION AND PRECISION
Both anterior and posterior hip replacements can be performed using various techniques and surgical approaches. Surgeons may utilize minimally invasive techniques, computer-assisted navigation, or robotic assistance to enhance precision and outcomes. The choice of technique depends on factors such as the patient’s anatomy, the surgeon’s experience, and the availability of technology in the operating room.
Posterior Approach
- Technique allows the surgeon full visualization if the hip cup and femur.
- No intraoperative x-rays needed.
- Very low risk of fracture due to easier exposure.
- When performed with the Mako Robotic-Arm there is a high-degree of precision of implant placement to recreate the patient’s natural anatomy.
Anterior Approach
- Technique allows excellent visual exposure of hip cup, but challenging exposure of femur requiring muscle and capsule release.
- Higher risk of femur fracture due to more difficult exposure.
- Intraoperative x-rays are often used to confirm placement of the implant due to less visual exposure.
MUSCLE PRESERVATION
One of the distinguishing features of the anterior approach is its emphasis on muscle preservation. By accessing the hip joint through natural muscle intervals, surgeons can minimize damage to surrounding tissues, potentially leading to faster recovery and improved function. In contrast, posterior hip replacements typically require cutting through muscles and tendons, which can result in longer recovery times and temporary weakness.
Posterior Approach
- The main incision goes through the gluteus maximus and will heal without repair.
- Muscles that are used to externally rotate the hip are detached during the procedure and later reattached to bone and will heal without complication.
Anterior Approach
- This procedure is not entirely muscle sparing. Due to risk of nerve damage, the incision enters the compartment of the tensor fascia latae muscle to expose the hip safely.
- The indirect head of the rectus femoris is released to allow entry into hip.
- External rotator muscles are cut and are not reattached during this approach.
- Most surgeons cut and do not repair the joint capsule.
NERVE DAMAGE
Nerve damage is a potential complication of both anterior and posterior hip replacements, although the risk may vary depending on the surgical approach. In anterior hip replacements, the femoral nerve is at risk due to its proximity to the surgical site. Surgeons must exercise caution to avoid damaging the nerve, which can lead to weakness or numbness in the leg.
In posterior hip replacements, the risk of nerve damage is generally lower, as nerves are less exposed during surgery. However, damage to the sciatic nerve, which runs close to the hip joint, is still possible and can result in pain, weakness, or sensory changes in the leg.
Posterior Approach
- Very small (less than 1%) risk of sciatic nerve damage from excessive retraction during surgery.
Anterior Approach
- Higher risk of injury to the lateral femoral cutaneous nerve, which may cause numbness in the outer thigh.
PRECAUTIONS
Patients undergoing anterior or posterior hip replacement surgery must follow specific precautions to optimize their outcomes and minimize complications.
Posterior Approach
- Low risk of dislocation when performed by a specialty-trained surgeon with a high volume of hip replacement.
- Discuss with your surgeon – some do not have post-operative precautions with this procedure.
Anterior Approach
- Low risk of dislocation when performed by a specialty-trained surgeon with a high volume of hip replacement.
- Dislocations are usually anterior and can occur with external rotation of the leg during any activity.
POST-OPERATIVE EXPERIENCE
After hip replacement surgery, the majority of our procedures are conducted on an outpatient basis, primarily at Bend Surgery Center and Cascade Surgicenter, unless patients are deemed unfit for ambulatory surgery. In some cases, joint replacement surgeries performed at St. Charles also facilitate same-day discharge whenever possible.
Patients will gradually increase their activity levels under the guidance of a healthcare professional, starting with gentle exercises and progressing to more strenuous activities as tolerated. Regular follow-up appointments with the surgeon will monitor the healing process and address any concerns or complications that may arise.
Posterior Approach
- At The Center, this procedure is most often performed in an outpatient setting (returning home the same day) at Cascade Surgicenter or Bend Surgery Center.
- Postoperative complications are the same for both approaches, including risk to structures, blood clots, infection, death, anesthesia risks.
- The medical equipment required for recovery for both approaches is the same. You may need a front-wheeled walker, cane, leg lifter, grab bars, and an elevated toilet seat.
Anterior Approach
- This procedure is also most often performed at an outpatient surgery center such as Cascade Surgicenter and Bend Surgery Center.
- Postoperative complications are the same for both approaches, including risk to structures, blood clots, infection, death, and anesthesia risks.
- The medical equipment required for recovery for both approaches is the same. You may need a front-wheeled walker, cane, leg lifter, grab bars, and an elevated toilet seat.
What is the difference between inpatient and outpatient surgery?
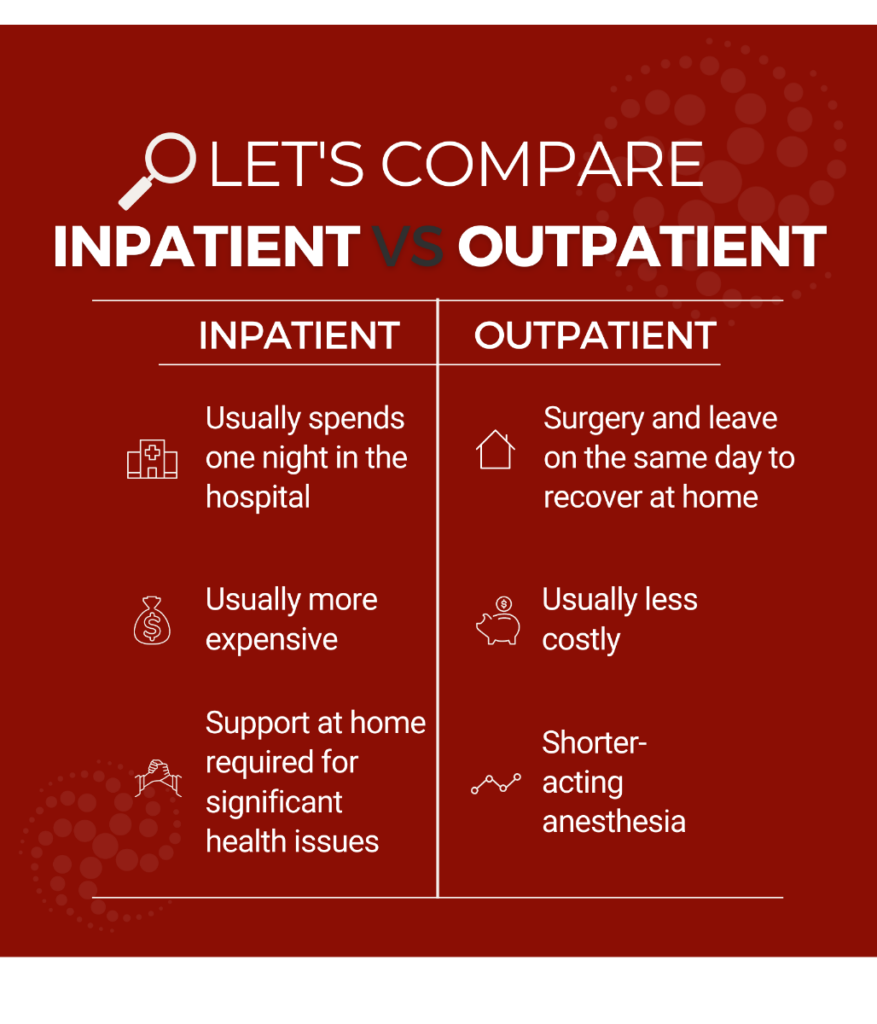 Orthopedic surgeon specializing in total hip replacements, Dr. James Hall, talks about the benefits and risks of outpatient total joint replacement in this video.
Orthopedic surgeon specializing in total hip replacements, Dr. James Hall, talks about the benefits and risks of outpatient total joint replacement in this video.
RETURN TO ACTIVITY
The timeline for returning to activity following hip replacement surgery varies depending on the surgical approach, the patient’s overall health, and the presence of any complications. In general, patients undergoing anterior hip replacement may experience a faster recovery and earlier return to normal activities due to the muscle-sparing nature of the procedure.
Patients undergoing posterior hip replacement may have a longer recovery period, as they may need more time to regain strength and mobility after the surgery. However, with diligent rehabilitation and adherence to postoperative precautions, most patients can expect to resume their favorite activities within a few months of surgery.
Posterior Approach
- Sedentary work – 2 weeks
- Light activity (walking, stationary bike, etc.) – 6 weeks
- Physical Work – 6-16 weeks
- Sports – 3 months
Anterior Approach
- Sedentary work – 2 weeks
- Light activity (walking, stationary bike, etc.) – 4-6 weeks
- Physical Work – 6-16 weeks
- Sports – 3 months
- Typically discontinue the use of walking device 1-3 weeks sooner than posterior approach.
Anterior and posterior hip replacements are two commonly performed surgical approaches for treating hip arthritis and injuries. Each approach has its own set of benefits and considerations, and the choice between them should be made in consultation with a qualified orthopedic surgeon.
By understanding the differences between anterior and posterior hip replacements, patients can make informed decisions about their treatment options and work towards an improved quality of life.
We’ve put together a free guide to help you better understand joint replacement preparation, orthopedic surgery, and recovery. If joint replacement surgery is the best solution for you, The Center’s orthopedic surgeons and support staff are ready to help you prepare for surgery and plan for a successful recovery. Click below to sign up and receive our free joint replacement guide.





