
Trigger finger, or “stenosing tenosynovitis” can often occur without experiencing a single injury. Trigger finger occurs when the flexor tendon becomes irritated and begins to thicken, eventually creating nodules making it difficult for the joint to bend and straighten. When the tendon is lengthening, it becomes momentarily stuck then quickly pops out into extension.
Learn more from Dr. Christopher Healy in this short video covering the anatomy of the finger, the causes of this painful condition, and possible treatment options. Dr. Healy is a fellowship-trained orthopedic surgeon, specializing in shoulder, elbow, wrist, hand, and trauma and fracture care. He enjoys the new and interesting challenges each day presents. Whether he is piecing together a fractured arm after an accident, seeing patients in clinic, or performing routine hand surgeries, every day is dynamic and immensely satisfying. What drives Dr. Healy the most is helping people and getting them back to what they love.
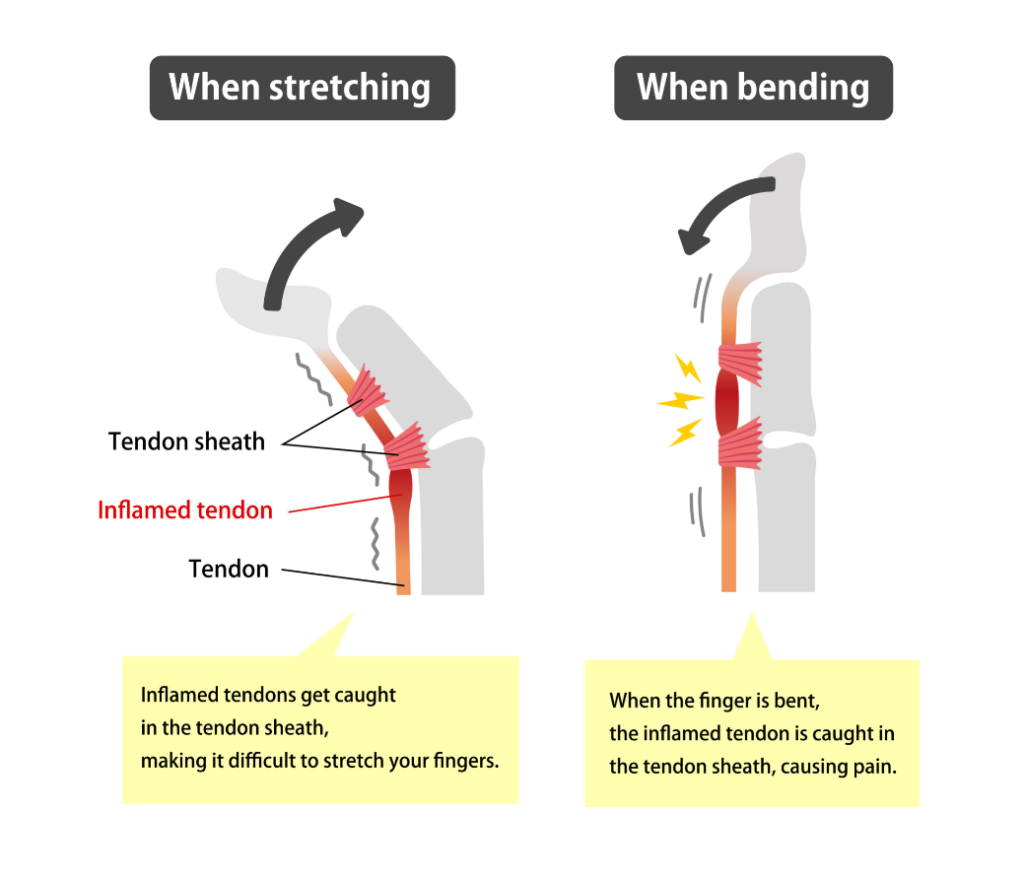
Trigger finger or stenosing tenosynovitis is a common condition seen by hand surgeons. It’s caused by swelling in the flexor tendons, which bend your fingers into your palm. Sometimes if the tendon is too swollen, it can cause the finger to get stuck and be very painful when you try and straighten it. Trigger finger can occur after a period of overuse, but can also have an insidious onset without a history of overuse injury of the hands. It occurs because the flexor tendons at the base of your finger enter a series of pulleys or tunnels, and the swollen tendon can get caught on the edge of the tunnel as you bend and straighten your finger. When the swollen tendon gets stuck on one side of the tunnel, patients often have to force their finger straight, which can be very painful.
It is common for catching or locking of the digit to be worse at night or in the morning while the tendon is more swollen. This is because when you sleep at night, tendons tend to swell a little bit more, and the swelling may resolve throughout the day, causing less catching or locking of your fingers. Trigger finger is very common. It is associated with diabetes, rheumatoid arthritis, and amyloidosis. However, trigger finger occurs frequently in patients without a history of these conditions.
Typically, there are four stages of a trigger finger. Initially, the patient may have tenderness to palpation at the base of their finger at the level of the first pulley or entrance to the tunnel. Next, the patient may notice that their finger has a catching sensation as they flex and extend their finger. Third, the patient may experience locking of the finger where they have to manually straighten their finger. And this is usually associated with a painful pop. Finally, when the inflammation is very severe, the finger will remain fixed and locked in an extended position. At this point, it is often too painful for the patient to bend their finger into their palm.
If you begin to experience symptoms similar to a trigger finger, you can first try at home care by resting, icing, and stretching the finger. Taking nonsteroidal anti-inflammatory drugs, such as ibuprofen or aspirin may also help reduce pain. If your pain won’t go away or gets worse, then it may be time to make an appointment with a hand surgeon to be properly diagnosed. Often trigger finger can be treated successfully without surgery. The typical first line of treatment is a steroid injection to the affected finger. The injection decreases the amount of inflammation within the tendon. Therefore, allowing the tendon to glide more smoothly through the tunnel. Generally, two out of three patients will have a successful result from the steroid injection and no further treatment may be necessary. Sometimes the steroid injection may last for several months and another steroid injection can be administered to the area as symptoms recur.
If the finger continues to trigger after two to three steroid injections, or if the injection does not provide long-lasting relief, your surgeon may recommend surgical release of the A1 pulley. Surgery involves cutting the roof of the tunnel, which allows the tendon to glide more smoothly. A trigger finger release can typically be performed under just local anesthetic with minimal discomfort following surgery.





