
What is arthritis?
Arthritis is the result of inflammation in one or more joints. This inflammation can cause pain, swelling, and stiffness in various joints within the body and can even lead people to replace their weight-bearing joints because the arthritis has interfered with their every day activity level. This can be particularly true with arthritis felt in the knee, one of the more common areas where arthritis can occur. Depending on how bad the pain is, it can interfere with daily activities people enjoy and can keep them from pursuing an active life.
Causes of Knee Arthritis: Who is Affected?
- Age: The risk of developing knee arthritis increases with age. The wear and tear on joints in older adults can lead to the breakdown of cartilage.
- Genetics: Some people may have a genetic predisposition to developing arthritis. If their parents or grandparents had arthritis, they may be more likely to develop it as well.
- Gender: Women are more likely than men to develop knee arthritis, especially after the age of 50.
- Obesity: Carrying excess weight puts extra stress on the knee joints. This can accelerate the breakdown of protective cartilage and increase the risk of developing arthritis.
- Previous Joint Injuries or Surgeries: People who have had previous knee injuries or surgeries, such as a torn meniscus or ligament, are at higher risk for developing arthritis in the affected knee.
- Joint Overuse or Misuse: Activities that involve repetitive stress on the knees, such as certain sports or occupations, can contribute to the development of knee arthritis over time.
- Muscle Weakness or Imbalance: Weak or imbalanced muscles around the knee joint can lead to abnormal stress on the joint, potentially accelerating the development of arthritis.
- Inflammatory Conditions: Conditions like rheumatoid arthritis, gout, or other autoimmune disorders can lead to inflammation in the joints, including the knees.
- Bone Deformities: Congenital or acquired bone deformities around the knee joint can alter the distribution of weight and pressure on the joint, potentially leading to arthritis.
- Metabolic Disorders: Conditions like hemochromatosis (excess iron in the body) and Wilson’s disease (copper buildup) can lead to arthritis.
- Infection or Trauma: Infections in the joint or significant trauma to the knee can lead to the development of arthritis.
It’s important to note that while these factors can contribute to the development of knee arthritis, it’s a complex condition and often involves a combination of genetic, environmental, and lifestyle factors. Additionally, not everyone with these risk factors will develop arthritis, and some individuals without these risk factors may still develop the condition. If you suspect you have knee arthritis or are experiencing knee pain, it’s important to consult a healthcare professional for proper diagnosis and treatment.
What is the Knee Joint?
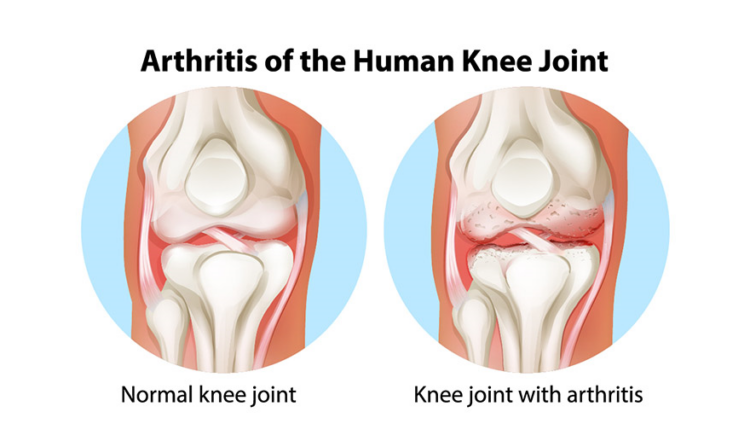
The knee joint is one of the largest and most complex joints in the human body. It serves as a pivotal point of connection between the thigh bone (femur), the shinbone (tibia), and the kneecap (patella). These bones come together in a specialized arrangement that allows for a wide range of movements, including flexion (bending), extension (straightening), and a degree of rotation.
- Bones that Form the Knee Joint:
- Femur (Thigh Bone): The femur is the longest bone in the human body and forms the upper part of the knee joint. Its rounded end, known as the femoral condyle, articulates with both the tibia and the patella.
- Tibia (Shinbone): The tibia is the larger and stronger of the two lower leg bones. It forms the lower part of the knee joint and supports the weight of the body. The top of the tibia, called the tibial plateau, interfaces with the femoral condyles.
- Patella (Kneecap): The patella is a small, triangular bone that sits in front of the knee joint. It glides over the femoral condyles during movements and provides leverage for the muscles that straighten the knee.
- Cartilage:
Within the knee joint, there are specialized tissues called cartilage. Cartilage is a firm, smooth, and slippery substance that covers the ends of bones. It acts as a shock absorber and reduces friction between bones during movement. In the knee joint, there are two types of cartilage:
-
- Articular Cartilage: This type of cartilage coats the surfaces of the femur, tibia, and the back of the patella. It allows the bones to glide smoothly against each other during movement.
- Meniscal Cartilage: The menisci are two C-shaped pieces of cartilage that sit between the femur and tibia. They act as shock absorbers and help distribute weight evenly across the joint.
- Synovial Fluid:
Surrounding the knee joint, there is a thin, viscous fluid known as synovial fluid. This fluid is secreted by the synovial membrane, a thin lining within the joint capsule. It serves multiple crucial functions:
-
- Lubrication: Synovial fluid lubricates the joint, reducing friction between the cartilage surfaces during movement.
- Nutrition: It provides nutrients to the avascular (without direct blood supply) cartilage, aiding in its maintenance and repair.
- Shock Absorption: The fluid’s viscosity helps absorb shocks and impacts on the joint.
- Waste Removal: Synovial fluid also helps remove waste products from the cartilage.
Together, these components – bones, cartilage, and synovial fluid – work together to facilitate smooth and pain-free movement within the knee joint. When any of these elements are compromised, it can lead to conditions like knee arthritis.
Types of Arthritis
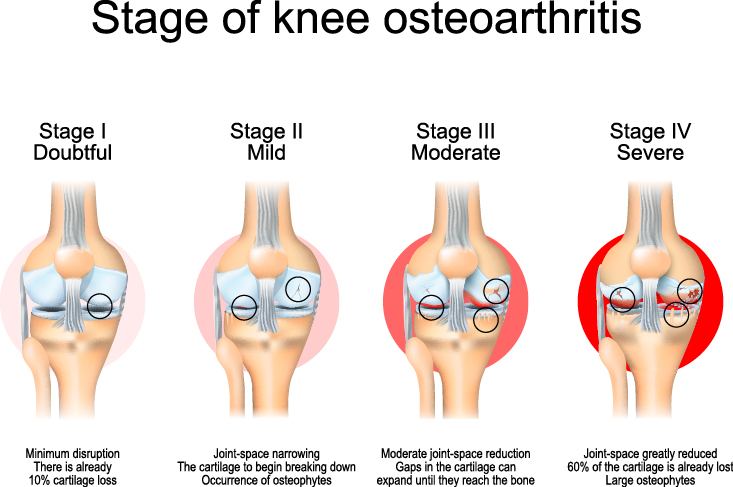
Not all types of arthritis are created equal. In fact, there are more than 100 different forms of arthritis. However, the two more common types of arthritis include osteoarthritis and rheumatoid arthritis. Osteoarthritis, which is known as a degenerative joint disease or “wear-and-tear” type of arthritis, is commonly found in the knee. It is rare for osteoarthritis to be found in younger people. It is more commonly found in people 50 years of age and older.
Why is osteoarthritis causing you so much pain?
Your joints contain cartilage between the bones to act as a protective cushioning. Osteoarthritis is the cartilage wearing away, becoming frayed and rough. When the protective space is compromised, bone on bone rubbing will produce painful bone spurs. The development of knee osteoarthritis can occur slowly, and the pain will worsen over time.
Rheumatoid Arthritis
Unlike osteoarthritis which can occur in a single joint, rheumatoid arthritis usually affects the same joint on both sides of the body. Known as an autoimmune disease, rheumatoid arthritis attacks multiple joints throughout the body, resulting in pain and stiffness. This autoimmune disease causes a person’s immune system to attack its own tissues, damaging healthy tissue such as cartilage and ligaments, and softening bone.
Posttraumatic Arthritis
After a traumatic injury occurs to a joint, posttraumatic arthritis can develop. In areas like the knee, if a broken bone has damaged the joint surface, this could lead to arthritis in the knee joint years following the injury.
Symptoms of Arthritis
Pain and inflammation from arthritis generally develop over time. “Swelling certainly can be a symptom of arthritis. At some point you could have what are similar to potholes in your cartilage, or you could get popping, clicking, and catching in your knee. It may start to feel like bones are rubbing together, which is a common sign that it is time to seek treatment,” states knee specialist at The Center, Dr. Ekaterina Urch.
Other knee arthritis symptoms:
- The joint may become stiff and swollen, making it difficult to bend and straighten the knee.
- Pain and swelling may be worse in the morning, or after sitting or resting.
- Vigorous activity may cause pain to flare up.
- Loose fragments of cartilage and other tissue can interfere with the smooth motion of joints. The knee may “lock” or “stick” during movement. It may creak, click, snap or make a grinding noise (crepitus) or grating sensation.
- Pain may cause a feeling of weakness or buckling in the knee.
- Many people with arthritis note increased joint pain with changes in the weather.
How is Knee Arthritis Diagnosed?
Diagnosing knee arthritis involves a comprehensive approach. Initially, your orthopedic surgeon will gather your medical history and assess your symptoms, focusing on factors like pain, stiffness, and mobility limitations. A thorough physical examination of the knee joint will be conducted, evaluating range of motion, stability, and any signs of tenderness or swelling. X-rays provide detailed images of bone structures, revealing indicators like joint space narrowing and bone spurs. For a more in-depth view of soft tissues, an MRI may be ordered. Blood tests also help rule out other potential causes of joint issues. In some cases, joint fluid analysis may be performed to gather additional information. If necessary, further specialized tests or consultations with specialists may be arranged to confirm the diagnosis and plan appropriate treatment.
Nonsurgical treatment for Knee Arthritis
When a patient is ready to address their arthritis, treatment will first be approached from a nonsurgical standpoint. Our orthopedic doctors in Bend have a number of different nonsurgical options they will first discuss with their patients and have them try before considering surgical treatment options.
Some of these nonsurgical recommendations could help slow the progression of arthritis in the knee:
- Minimize activities that aggravate the condition, such as climbing stairs.
- Switching from high-impact activities (like jogging or tennis) to lower impact activities (like swimming or cycling) will put less stress on your knee.
- Weight loss can reduce stress on the knee joint, resulting in less pain and increased function.
Other nonsurgical options to help ease arthritis pain:
- Physical Therapy
- Assistive Devices
- Applying heat or ice, using pain-relieving ointments or creams, or wearing elastic bandages to provide support to the knee may provide some relief from pain.
What medications help relieve knee pain from arthritis?
There are many different types of drugs that can help treat arthritis of the knee. Different patients respond in different ways to medications, and because of this, a doctor works closely with their patients to determine which medications and dosages are safe and effective.
Some of these medications may include:
- Over-the-counter medications, non-narcotic pain relievers and non-steroidal anti-inflammatory medications. Like all medications, over-the-counter pain relievers can cause side effects and interact with other medications you are taking. Be sure to discuss potential adverse effects with your doctor.
- Another type of pain reliever is a nonsteroidal anti-inflammatory drug, or NSAID (pronounced “en-said”). NSAIDs, such as ibuprofen and naproxen, are available both over-the-counter and by prescription.
- Corticosteroids (also known as cortisone) are powerful anti-inflammatory agents that can be injected into the joint.
Surgical Treatment for Knee Arthritis
Should pain reach the point of disability for a patient and nonsurgical treatment is no longer effective, a doctor may recommend surgery to help restore function. As with all surgical procedures, there are some risks and possible complications with different knee procedures. Your doctor will discuss the possible complications with you before your operation.
Arthroscopy. During arthroscopy, doctors use small incisions and thin instruments to diagnose and treat joint problems.
Arthroscopic surgery is not often used to treat arthritis of the knee. In cases where osteoarthritis is accompanied by a degenerative meniscal tear, arthroscopic surgery may be recommended to treat the torn meniscus.
Cartilage grafting. Normal, healthy cartilage tissue may be taken from another part of the knee or from a tissue bank to fill a hole in the articular cartilage. This procedure is typically considered only for younger patients who have small areas of cartilage damage.
Synovectomy. The joint lining damaged by rheumatoid arthritis is removed to reduce pain and swelling.
Osteotomy. In a knee osteotomy, either the tibia (shinbone) or femur (thighbone) is cut and then reshaped to relieve pressure on the knee joint. Knee osteotomy is used with early-stage osteoarthritis that has damaged just one side of the knee joint. By shifting your weight off the damaged side of the joint, an osteotomy can relieve pain and significantly improve function in the arthritic knee.
Total joint replacement surgery or partial knee replacement (arthroplasty). The doctor will remove the damaged cartilage and bone, and then position new metal or plastic joint surfaces to restore function of the knee. The doctor and patient determine whether inpatient or outpatient knee replacement surgery will best fit the patient’s needs and abilities.
Arthritis of the Knee Prevention Tips
To prevent or manage knee arthritis, adopting a proactive approach and making lifestyle adjustments can be highly effective:
- Engage in regular, low-impact exercises like swimming, cycling, or walking to strengthen knee-supporting muscles.
- Prioritize exercises that target the quadriceps, hamstrings, and calf muscles for enhanced joint support.
- Incorporate stretching routines to preserve joint flexibility and reduce the risk of stiffness and discomfort.
- Wear well-fitting, supportive shoes with proper arch support to evenly distribute weight and minimize stress on knees.
- Minimize high-impact activities such as running or jumping to mitigate excessive wear and tear on the knees.
- Prioritize warm-up exercises before physical activity and cool down afterward to prepare muscles and prevent stiffness.
- Practice good posture to evenly distribute body weight and reduce unnecessary strain on the knees.
- Maintain a healthy weight to alleviate excess strain on the knees.
Consulting an orthopedic surgeon for personalized advice and treatment options is crucial, as individual circumstances may vary.Top of Form
Source: https://orthoinfo.aaos.org/
We’ve put together a free guide to help you better understand joint replacement preparation, orthopedic surgery, and recovery. If joint replacement surgery is the best solution for you, The Center’s orthopedic surgeons and support staff are ready to help you prepare for surgery and plan for a successful recovery. Click below to sign up and receive our free joint replacement guide. Stay informed about upcoming webinars and events, and gain valuable insights on leading a healthy, pain-free life from our experts by subscribing to our monthly newsletter. Click the button below to join!





