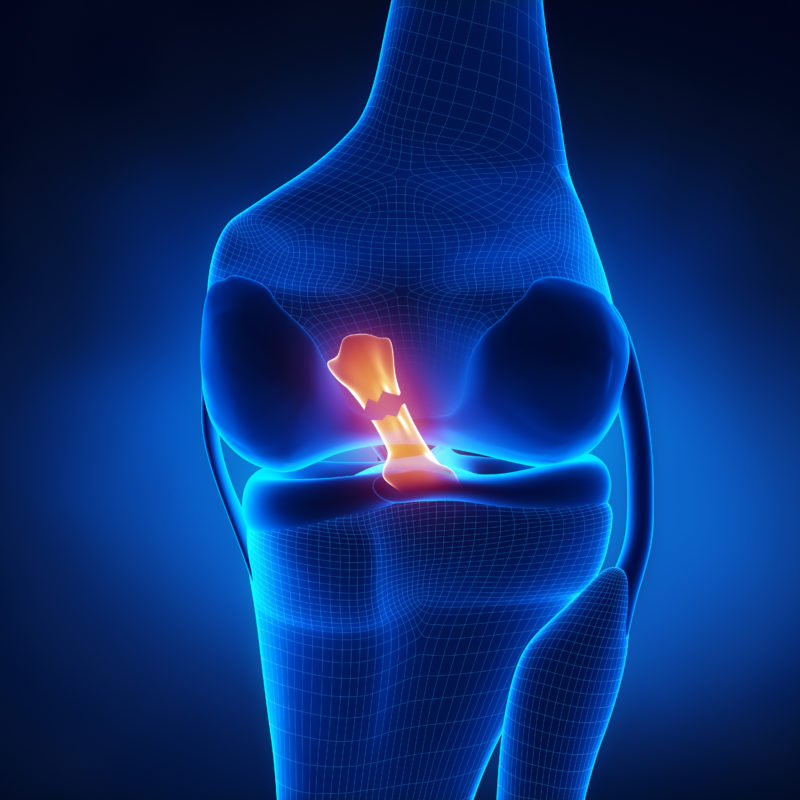
Once you and your orthopedic surgeon have decided to undergo surgery to reconstruct the anterior cruciate ligament (ACL) in your knee, you will need to choose which replacement graft to use. The torn ligament will not repair itself, nor can it be sewn together successfully. It must be replaced with a new tissue that will develop into a ligament over time. Choosing which graft is appropriate is not always an easy decision. There are pros and cons to each alternative. Your choices include your own tissue (autograft) or cadaveric tissue (allograft).
Autographs
The patellar tendon and hamstring autografts are the most common choices for ACL reconstruction. The patellar tendon runs from the knee cap (patella) to the lower leg bone (tibia). Surgeons have the most experience with this autograft and it is the most widely used. A vertical incision is made from the bottom of the patella to the top of the tibia. The middle third of the tendon is then cut, as well as the bony portions from the patella and tibia. The final autograft is made from the partial tendon and bones on either end. The bone on both sides allows for quicker healing of the graft.
Benefits:
- Orthopedic surgeons have the most experience with this procedure
- Strongest graft concerning initial fixation
- Quicker return to full athletic participation, typically 5-6 months
Risks:
- Increased chance of pain or discomfort while kneeling
- More painful due to harvesting the tendon and bone portions
- There is an extra incision where the graft is harvested
- Increased risk for patellar fracture
- Increased risk for patellar tendonitis
Although called the hamstring autograft, the tendons associated with this graft are not technically part of the hamstring. The semitendinosis tendon and the gracilis tendon are removed from a small incision just below and near the inside of the knee. This autograft has no bony portions and uses two tendons.
Benefits:
- Least amount of post-operative pain
- Easier rehabilitation in regards to quadriceps activation
- Quicker return to activities of daily living
- No extra incision is required. The same incision is used to place the fixation hardware.
Risks:
- The fixation is not as strong initially. Caution is advised with rehabilitation.
- Some hamstring weakness may be noted
- Return to full athletic participation is slower, 6-7 months
- There is no hamstring activation for at least four weeks to allow the harvest site to heal
- Increased risk for hamstring strain/tenderness
Allografts
Allografts provide another option for ACL reconstruction. The tissue is harvested from a cadaver, so there are no complications from taking the tissue from your own body. The most common choices are Achilles tendond, quadriceps, anterior tibialis tendon, and patellar tendon. The decision on which allograft option to use is based on what is available and surgeon preference. Overall, the grafts are just as strong if you follow the specific rehabilitation protocol. Although donors are screened for communicable diseases, there is a risk of disease transmission associated with using graft tissue from a cadaver. There is a potential for viral transmission such as hepatitis or HIV.
Benefits:
- No pain or complications from harvesting the tissue
- Fastest return to activities of daily living
- Smaller incision on the medial tibia
Risks:
- Potential risk of viral transmission (chance of HIV transmission is 1 in 1.8 million)
- Return to full athletic activities is generally 6-7 months
- Higher re-tear rate in younger competitive athletes
Choosing which graft to use for ACL reconstruction is highly individualized for each patient. Discuss your lifestyle and the risks and benefits with your orthopedic surgeon to determine the best course of action to reach your goals.